Call for immunology to return to the wild
A multidisciplinary research team from more than 10 universities and research institutes has outlined how integrating a more diverse set of species and environments could enhance the biomedical research cycle.
The viruses that cause COVID-19, AIDS, Ebola, and rabies – among others – all made the lethal jump from wildlife into humans.
In an article published in Science, the researchers argue that understanding how the immune system works in animals that live with coronaviruses in a natural environment, such as bats, can give us direction for developing treatments and vaccines to protect humans from viruses.
Lead author Dr Andrew Flies from the Menzies Institute for Medical Research at the University of Tasmania, says this is not a new concept.
“The very first vaccine arose from observing people interacting with animals in a real-world environment. Specifically, milkmaids who acquired a mild cowpox infection from cows were protected from the deadly smallpox. That observation led to the idea of inoculating people with non-lethal viruses to protect them from deadly viruses. This type of discovery can only be made by studying new species in variable environments.”
Modern research relies heavily on mouse experiments in laboratory settings, which limits the scope for this type of ground-breaking discovery.
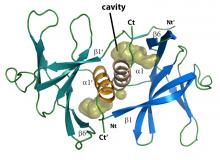
An example of a long-term payoff from stepping out of the lab is the discovery of a new class of antibodies, often referred to as nanobodies, in camels. Easier and faster to make than traditional antibodies used in biomedicine, camel-derived nanobodies are playing an important role in biomedical research, including the global COVID-19 response.
“We are really excited to see how our initial group discussions held at the first Australian Wild and Comparative Immunology (WACI) workshop led to publishing a Perspective article in a world leading journal,” said co-author Dr Jérôme Le Nours, from the Biomedicine Discovery Institute at Monash University, who was co-organiser of the WACI meeting.
Associate Professor Anne Peters, Monash University, co-author and consortium collaborator, added: “There are many excellent wildlife and disease ecologists, veterinarian scientists and immunologists in Australia, and beyond. We hope that our contribution will inspire them to seek mutually beneficial, inter-disciplinary collaboration”.
WACI Consortium collaborator and co-author Associate Professor Julie Old from Western Sydney University said it’s important for immunology research to include more diverse species.
“If we want to evolve our understanding of the immune system, and potentially get ahead of any future pandemics, the research community needs to expand. We need to broaden our scope, and bring new species and new environments into the research paradigm.”
Associate Professor Michelle Power from Macquarie University said: ‘‘Realising wild immunology needs initiatives like the WACI Consortium that harness the wide expertise of scientists and diverse technologies within individual. The risks of emerging infectious diseases are not going away. We need new ideas, new tools and dynamic collaboration to address them”.
The Director of the Menzies Institute for Medical Research, Distinguished Professor Alison Venn, said new technology has broken down research barriers to integrating new species and environments into the research cycle.
“Proactive investment in wild immunology can stimulate discoveries with real-world applications for human and veterinary medicine and conservation. It could help us prepare for the next pandemic.”
Read the Rewilding immunology article published in Science.
Learn more about how integrating a more diverse set of species and environments could enhance the biomedical research cycle by watching the video below.