Congrats Ben and team on your Nature paper
Structure of a key “trigger” of the immune response solved
An international collaboration, involving researchers from Monash University and the University of Oxford, has led to a breakthrough in our understanding of how immune responses are started. The study has just been published in Nature.
The human immune system comprises multiple important white blood cells (i.e., lymphocytes) including B cells and T cells that fight off infections and cancers. Basic discoveries leading to an understanding of how lymphocytes function have led to the development of immunotherapies and vaccines.
There are two types of T cells in humans, called αβ T-cells and γδ T cells, each of which expresses on their surfaces either an αβ T cell receptor (TCR) or a γδ TCR, respectively. In 1957, Frank Macfarlane Burnet, a famous Australian immunologist, predicted the existence of these receptors and speculated that they would “trigger” clonal lymphocyte expansions, producing enough cells to fight off infections. We now recognize that TCRs have the pivotal role of recognising molecules derived from foreign pathogens or tumours. While less is known about γδ T cells than αβ T cells, they are emerging as key players in immune defence and are becoming increasingly important for immunotherapy.

Figure. The image shows the unusual, flexible arrangement of the γδ TCR versus the αβ TCR. B-cell receptor is expressed by antibody-making B-cells.
The team determined the molecular structure of the TCR found on the surface of γδ T cells using cryogenic electron microscopy. This technically demanding project took over a decade from conception to completion and was made possible by the expertise within the Monash Ramaciotti Centre for Cryo-Electron Microscopy.
The new structure unexpectedly showed that the γδ TCR is remarkably flexible, in stark contrast to relatively rigid αβ TCRs. The work also showed that the γδ TCR is very likely the more primeval receptor and completes the initial structural analysis of Burnet’s “trigger” receptors, alongside companion paper also published in Nature.
“This flexibility is key to the ability of the γδ TCR receptor to recognise a wide array of binding partners, which underscores the unique role it plays in the human immune system”, Dr Benjamin Gully of the Monash Biomedicine Discovery Institute, co-first author of the study stated.
According to Professor Simon Davis, from Oxford University and joint senior author of the study, γδ T-cells are becoming increasingly important therapeutically.
“The new structure helps constrain theories of how TCRs trigger lymphocytes, and should be helpful, especially, for re-engineering TCRs and optimising their use in the clinic” he said.
The authors would like to acknowledge support from the Australian Research Council Discovery Program which made this basic research project possible.
Read the full paper in Nature: Structure of a fully assembled γδ T-cell antigen receptor.
DOI: 10.1038/s41586-024-07920-0

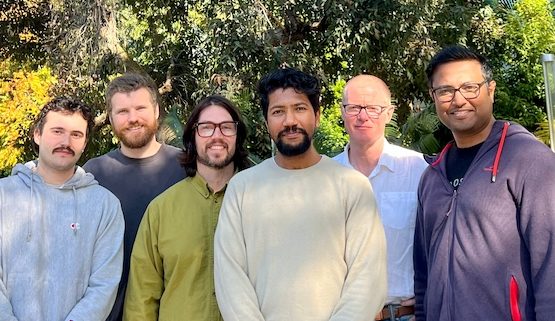
Some of the Monash University co-authors on the Nature publication (left to right): Liam Rashleigh, Michael Rice, Dr Benjamin Gully, Dilshan Gunasinghe, Professor Jamie Rossjohn, Hari Venugopal.